Blank Do Not Resuscitate Order Template for Washington State
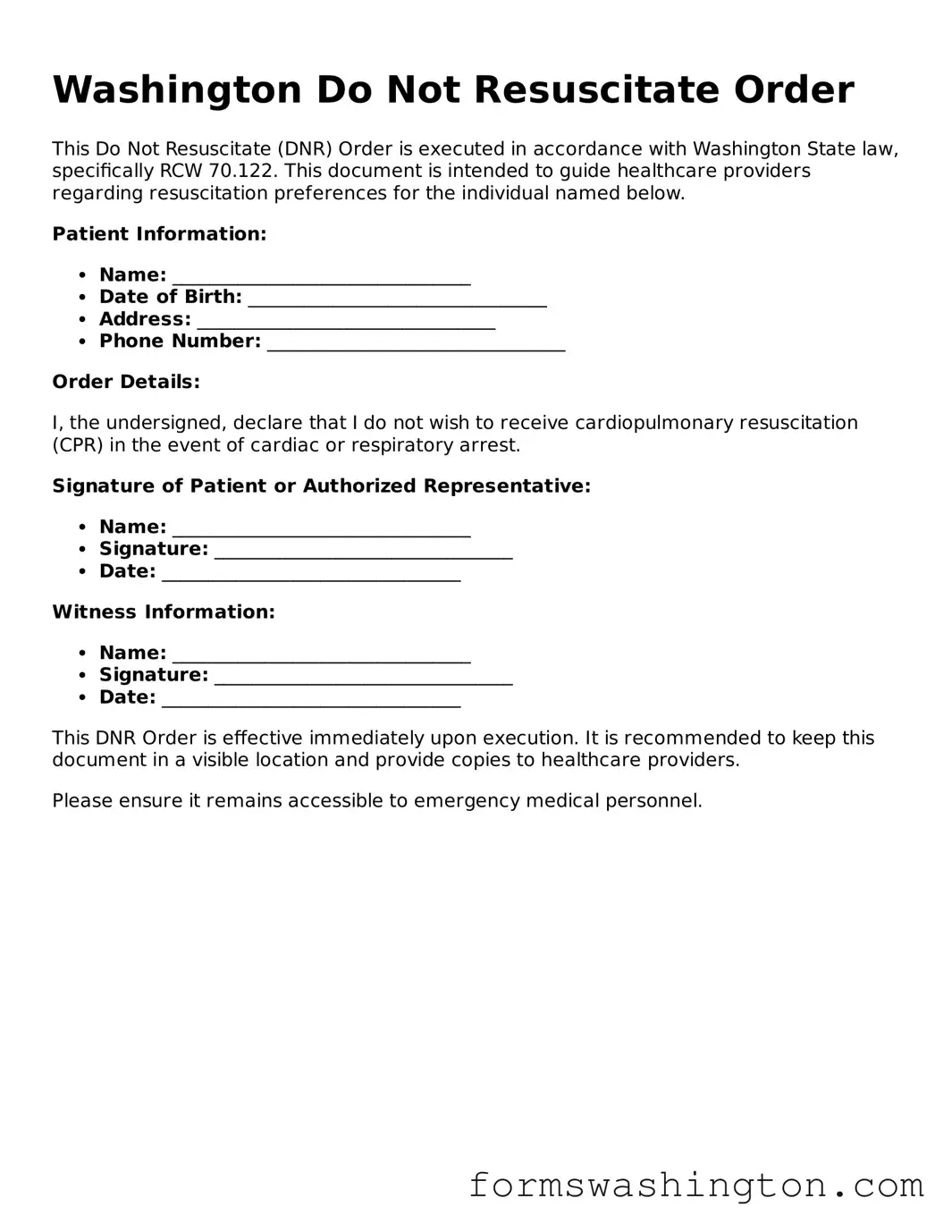
The Washington Do Not Resuscitate (DNR) Order form is an essential legal document for individuals who wish to express their preferences regarding medical treatment in critical situations. Designed to ensure that a person's wishes are respected, this form specifically addresses the desire to forgo resuscitation efforts in the event of cardiac arrest or respiratory failure. It is important to understand that a DNR order does not affect other types of medical care; it solely pertains to resuscitation. The form must be completed and signed by a qualified healthcare provider, along with the patient or their legal representative. In Washington, this document is recognized by all healthcare facilities and providers, making it crucial for anyone considering end-of-life care options. Additionally, individuals can carry a copy of the DNR order with them to ensure that their wishes are honored in emergencies. Understanding the nuances of the DNR form can empower individuals to make informed decisions about their healthcare, ensuring that their preferences are clearly communicated and respected by medical personnel.
Documents used along the form
The Washington Do Not Resuscitate Order (DNR) form is an important document for individuals who wish to specify their preferences regarding resuscitation efforts in the event of a medical emergency. Several other forms and documents may accompany the DNR to provide comprehensive guidance on a person's healthcare decisions. Below is a list of these related documents.
- Advance Directive: This document outlines an individual's preferences for medical treatment in situations where they are unable to communicate their wishes. It can include instructions on various types of care, not just resuscitation.
- Health Care Power of Attorney: This form designates a specific person to make healthcare decisions on behalf of an individual if they become incapacitated. The appointed agent can make choices based on the individual's wishes.
- Living Will: A living will provides instructions regarding medical treatment preferences, particularly at the end of life. It is often used to express wishes about life-sustaining treatments.
- Vehicle/Vessel Transfer and Reassignment Form (REG 262): This form is essential for transferring ownership of a vehicle or vessel in California, serving multiple functions including a bill of sale and odometer disclosure. For more detailed information, visit OnlineLawDocs.com.
- Physician Orders for Life-Sustaining Treatment (POLST): This form translates a patient’s treatment preferences into actionable medical orders. It is intended for individuals with serious illnesses or those nearing the end of life.
- Do Not Intubate (DNI) Order: This document specifies that a patient should not be intubated in the event of respiratory failure. It is often used in conjunction with DNR orders.
- Emergency Medical Services (EMS) DNR Order: This form is specifically designed for use by emergency medical personnel. It ensures that the DNR wishes are honored in pre-hospital settings.
- Patient Preferences Form: This document allows individuals to express their preferences regarding various medical treatments and interventions. It can be used to guide healthcare providers in decision-making.
- Organ Donation Consent Form: This form indicates an individual's wishes regarding organ donation after death. It can be included with end-of-life planning documents.
- Healthcare Proxy Form: Similar to a power of attorney, this form designates an individual to make healthcare decisions. It is often used in conjunction with advance directives.
These documents work together to ensure that an individual's healthcare preferences are respected and followed. It is advisable for individuals to discuss these forms with their healthcare providers and loved ones to ensure clarity and understanding of their wishes.
Misconceptions
Understanding the Washington Do Not Resuscitate (DNR) Order form is essential for individuals and families making end-of-life decisions. However, several misconceptions can lead to confusion. Here are seven common misconceptions:
- A DNR means that no medical care will be provided. Many people believe that having a DNR in place means a person will not receive any medical treatment. In reality, a DNR specifically addresses resuscitation efforts, such as CPR or the use of a defibrillator, but does not prevent other types of medical care.
- Only terminally ill patients need a DNR. While DNR orders are often associated with terminal illnesses, they can be appropriate for anyone who wishes to avoid resuscitation in the event of a cardiac arrest, regardless of their overall health status.
- A DNR is permanent and cannot be changed. This is not true. Individuals can change or revoke a DNR order at any time, as long as they are capable of making decisions about their medical care. It’s important to communicate any changes to healthcare providers.
- All healthcare providers are familiar with DNR orders. While many healthcare professionals are knowledgeable about DNR orders, not all may be fully aware of a specific patient’s wishes. It is crucial to ensure that the DNR is communicated clearly to all involved in the patient's care.
- A DNR order is the same as a living will. Although both documents relate to end-of-life decisions, they serve different purposes. A living will outlines a person’s preferences for medical treatment in various situations, while a DNR specifically addresses resuscitation efforts.
- Having a DNR means giving up on life. Some people mistakenly believe that choosing a DNR is a sign of giving up. In reality, it is a personal choice that reflects an individual’s values and wishes regarding the type of care they want at the end of life.
- DNR orders are only valid in hospitals. DNR orders are valid in various settings, including homes, nursing facilities, and other healthcare environments. It is essential to ensure that the order is recognized by all healthcare providers, regardless of the setting.
By addressing these misconceptions, individuals and families can make more informed decisions regarding DNR orders and ensure that their healthcare preferences are respected.
Check out Some Other Templates for Washington
Power of Attorney Washington State Pdf - The document can be tailored to include specific tasks or responsibilities you want your agent to handle.
When engaging in the sale of a recreational vehicle, it is crucial to utilize the appropriate documentation, such as the Texas RV Bill of Sale, which can be found at https://topformsonline.com/texas-rv-bill-of-sale/. This document not only transfers ownership from the seller to the buyer but also serves as an important safeguard for both parties involved in the transaction.
Do Snowmobiles Have Titles in Washington State - A necessary document for financing a snowmobile purchase.
Dos and Don'ts
When filling out the Washington Do Not Resuscitate Order form, it’s crucial to approach the process with care and attention. Here are some important dos and don’ts to consider:
- Do ensure that you fully understand the implications of a Do Not Resuscitate Order. This decision can significantly impact medical treatment.
- Do consult with your healthcare provider before completing the form. They can provide valuable insights tailored to your health situation.
- Do sign and date the form in the presence of a witness, if required. This step helps to validate your wishes and ensure they are legally recognized.
- Do keep copies of the completed form in accessible locations. Share it with your healthcare provider and loved ones to ensure everyone is informed.
- Don’t rush through the form. Take your time to read each section carefully and make sure all information is accurate.
- Don’t fill out the form without considering your values and wishes regarding end-of-life care. This is a deeply personal decision.
- Don’t assume that a verbal agreement is sufficient. Written documentation is essential for your wishes to be honored.
- Don’t forget to review the form periodically. Changes in your health or personal circumstances may require updates to your order.